Editor’s note: In a five-part series, Jayme Doll explores the struggles some Albertans experience in getting their reproductive conditions recognized and treated. Part 1 is in the video player above. The rest of the series will be added as it airs the week of March 10-14.
There are no shortage of labels and euphemisms for it: time of the month, aunt flo, shark week, code red, or, as most of us know it — periods.
A natural, love-hate reality bonding together half of the world’s population.
For some, menstruation is a life-giving gift —for others it can be a week or more of sheer hell.
For far too long, many women have been sitting in silent, crippling agony every month that far exceeds the boundaries of normal.
“You always have those that say, ‘Oh it’s just bad cramps, oh it’s just a tummy ache.’ But I knew my body and I knew something was wrong,” said Canmore’s Katie Leaf.
“I feel so often we are discredited, told we are fine or it’s not much pain, ignored, passed on.”
“It’s really frustrating, I feel the anger of not being listened to,” she said.
Katie’s pain started as a teenager, she never gave up advocating for herself. At 21 years old, she was diagnosed with endometriosis and polycystic ovarian syndrome.
“I have landed in the hospital quite a few times — the pain is blinding. You can’t move, you can’t think straight, can’t see straight.”
It took 23 years for Laura McDonald to get a diagnosis for her excruciating a period pain, also due to endometriosis.
“I’ve been told that the pain was in my head that I imagined the pain at times,” she said. “I had health anxiety and was referred to counseling I had have to do cognitive behavior therapy.
“I didn’t know what was wrong with me.”
Both polycystic ovarian syndrome (also called polycystic ovary syndrome, or PCOS) and endometriosis impacts 1 in 10 people of reproductive age.
PCOS is a hormonal imbalance disorder that causes irregular cyst growth, the presence of extra male hormones (which cah cause acne or unwanted facial hair) and irregular periods. It can cause infertility issues.
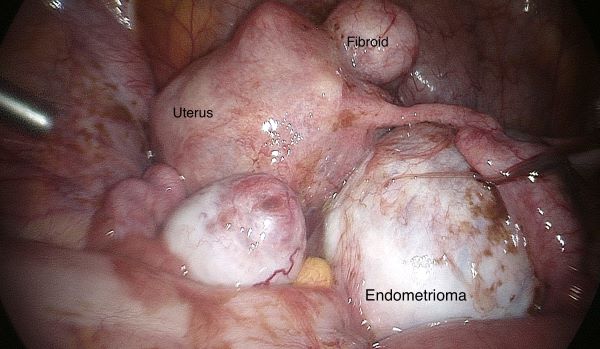
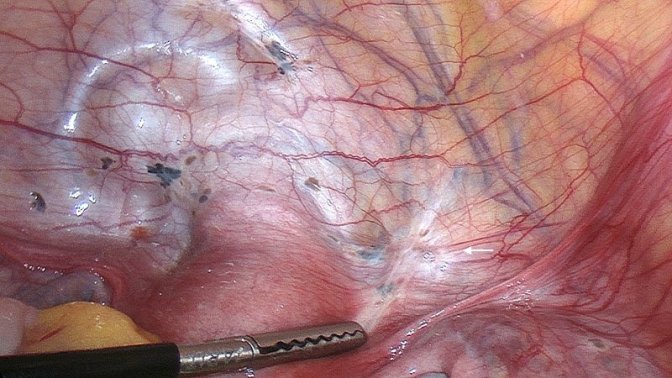
With endometriosis, cells normally found in the lining of the uterus spread to other parts of the body, causing debilitating pain, heavy bleeding and at times, also infertility.
Currently, the gold standard to being diagnosed with endometriosis is through laparoscopic surgery, where surgeons will often then try to excise the endometrial tissue growing outside the uterus and repair any damage.
But there is no guarantee of it not growing back. Both Katie and Laura, now in their 30s, have had surgery — Katie has underwent it multiple times.
“I remember talking to the surgeon in my post-op and he used the word ‘infertile’ and as a 21-year-old woman, I always wanted to be a mom. That was really hard to hear,” Katie said.
Both women agree the diagnosis helped validate their pain and finally opened more doors to help manage it, many are still waiting.
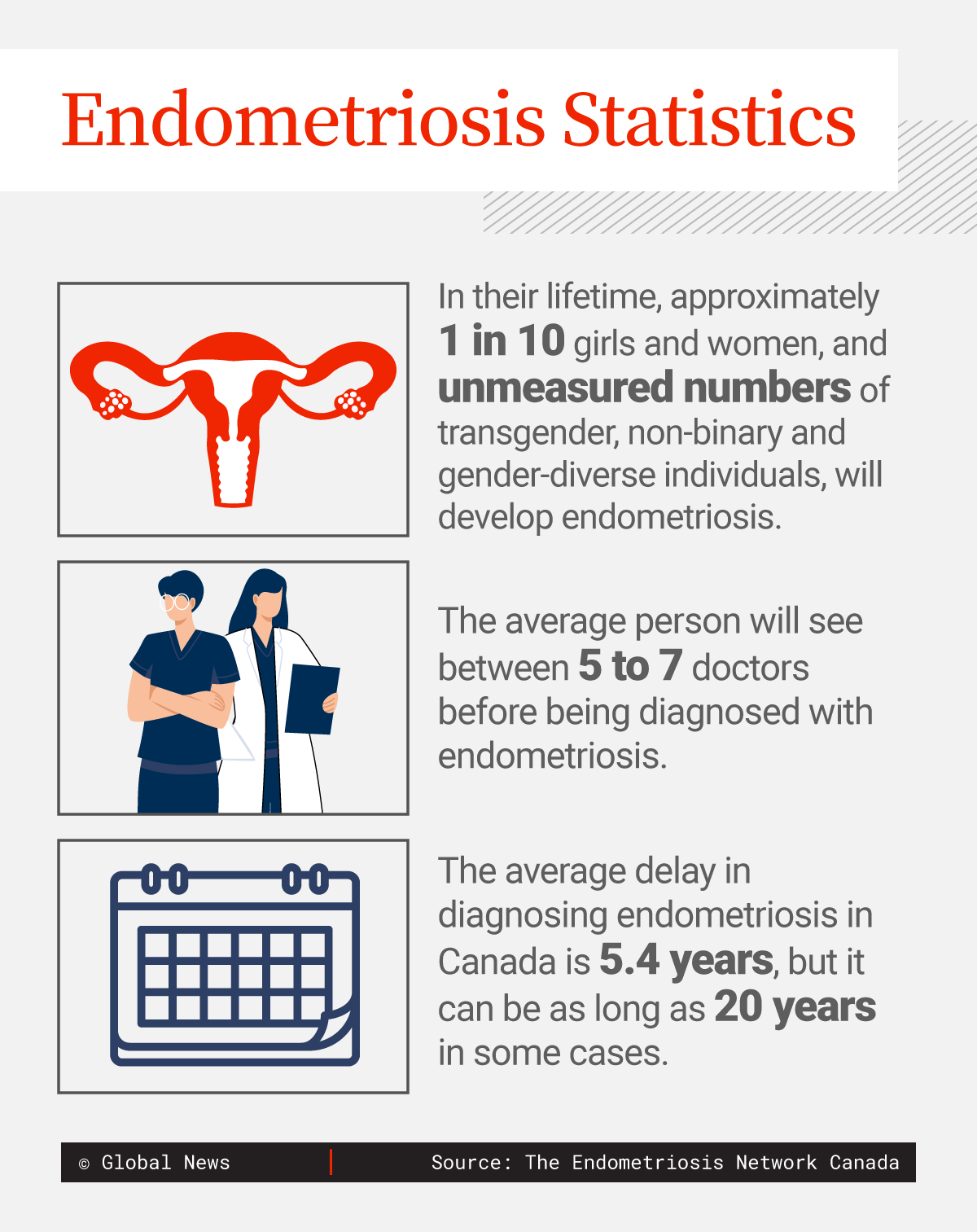
Endometriosis Statistics.
Infographic by Fasai Sivieng
“I just physically can’t get out of bed, I can’t move, so it’s stopped me in a lot of ways from just living,” said Edmonton’s Rose Plican.
The 19-year-old NAIT student’s debilitating periods have forced her to hit pause on her studies many times.
“It’s a lot of men in my class and so you are sitting there, you are dying in class — and they are like, ‘You ok? What’s going on with you?’
“How am I supposed to explain to a bunch of dudes that, like, I’m on my period I just need to go home?”
“It’s embarrassing, especially if you flow through,” she added.
Rose is on a two-year waiting list to see a gynecologist and has been waiting months for a pelvic scan.
“It’s an 8.5-year diagnostic delay worldwide, Canada is at 5.3 years I think that’s extraordinary,” said Carolyn Plican, Rose’s Mom, who is also a women’s health-care advocate.
Carolyn discovered a new technology created in the U.S. and now being used in the Middle East, UK and at one clinic in Canada.
It is a non-invasive diagnostic test for endometriosis called EndoSure that promises to take just 30 minutes.
Plican was so passionate about it and helping her daughter, she to her certification to use the technology.
“Suddenly when you are diagnosed, you know it’s not in your head so it gives you permission to let you know you need better strategies to manage pain or you need to be on a waitlist for laparoscopy to have it excised, if it’s affecting you really badly,” said Plican.
Over the past 10 years there have been huge advancements in minimally-invasive gynecological surgery, but women’s health specialists still face barriers.
“We are being empowered by our patients and we are finding our voice, but unfortunately we are playing catch up in a health-care system that has always equated gynecology with obstetrics and hasn’t recognized the power of what we can offer surgically,” said Dr. Liane Belland.
The Calgary surgeon has helped lead the charge in the field of minimally invasive and complex gynecological surgery. Her clinic can have as many as 700 new patients a year.
“The way that our current surgical time allocation is, there isn’t a priority on gynecologic care, there has never been a priority on gynecologic care,” said Belland.
“It’s difficult to listen to the struggles of people day in and day out — you want to help people and sometimes there are restraints, system restraints, OR waitlists.”
“Ideally you’d love to get everyone in the operating room, of course of you want everybody to afford the medical management you want to offer them, but that’s not the reality,” said Belland.
Gynecologist like Dr. Belland admits stigma still can be a barrier preventing patients from reaching out for help in the first place.
“A lot of people suffer in silence,” said Dr. Ari Sanders, a Calgary-based gynecological surgeon.
“When women are missing school because of pain, or when they are missing work because of bleeding that’s not normal, that should not be happening,” Sanders said.
Specialists said social media and support groups are helping to bring legitimacy to debilitating period pain that’s been brushed off forever as normal — something women just need to put up with.
Women in Calgary attend a support group for endometriosis, PCOS and fibroids in March 2925.
Global News
Laura McDonald started a support group to do just that. They meet on Mondays for tea and often invite health experts to answer questions. But hearing each other’s own personal stories is proving to be therapeutic.
“Endo is very isolating, navigating the medical system is isolating — so just coming together with other women who are experiencing this makes you feel less alone and pretty supported,” said Erin Ramsey, a group member.
The fight to unshackle debilitating periods from societal stigma is growing steam.
Change.org has numerous petitions lobbying for paid period sick days and even support with products. Some believe society as a whole has a role to play-in understanding the severity some face.
“I’m hoping that workplaces, schools things like that will come around a little more to accepting woman are cyclical and we do have to work with those cycles a little more to have optimal health,” said Many LeBlanc, A women’s health practitioner.
” Women should not have to just muscle on and grin and bear it,” said Dr. Belland.
Katie Leaf admits she has had to do it many times, but has found power in her own vulnerability — listening to her body and knowing when it’s ok to just rest.
She wants others to know they don’t have to suffer in silence alone.